Blog

Flip Flops and Feet
Flip flops are often a popular choice of footwear for many people. Flip flops allow your feet to breathe and give your toes the freedom of movement. They are easy to slip on and can be worn with virtually any style of clothing. Flip flops, however, despite their many benefits, can be detrimental for your foot health.
Despite their comfortableness, frequently wearing flip flops can create problems in the lower body over time. Issues mainly stem from the fact that people walk differently in flip flops compared to other footwear, such as sneakers. This is due to a change in one’s natural gait, which therefore creates stress in different parts of the body while hindering the body’s natural posture. Problems can also arise in the arches and balls of the feet. Flip flops provide little to no support to these areas.
Aside from long-term problems, flip-fops can also create short-term issues as well, such as ankle sprains and blisters. Weak materials that are flexible and bendable are generally used to manufacture flip flops. These materials make its wearers prone to both tripping and injuring their ankles. Flip flops can create blisters as the material rubs against the foot. People are much more at risk for infection while wearing flip flops due to their openness. This also makes it easier to scrape and cut the foot since there is a lack of protection. If these cuts are left untreated and uncovered, the risk then becomes greater.
To prevent the aforementioned occurrences, purchase a pair of flip flops that offer significant protection. The soles of the flip flops should not be floppy, but sturdy and firm, and should not significantly bend or wiggle when lifted from the floor. Flip flops made of high-quality materials will not be affected by this problem. While higher quality flip flops may be more expensive, they will last longer and provide better protection compared to a cheaper pair. Brand name flip flops sold from a quality manufacturer are a dependable option.
There is no problem in wearing your favorite pair of flip flops so as long as you do not wear them daily or for extended periods of time. Flip flops should be replaced every 3-4 months to ensure that they provide your feet with the best protection.
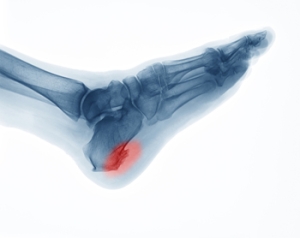
How Did I Get a Heel Spur?
A spur is a bony growth that may develop due to repetitive irritation or stress. As its name suggests, a heel spur develops on the heel bone or calcaneus. More specifically, it typically forms in one of two places on the heel bone. An inferior calcaneal spur forms underneath the heel bone and is associated with plantar fasciitis, a common ligament injury in the foot. A posterior calcaneal spur forms on the back of the heel bone and is associated with Achilles tendonitis. Heel spurs can be asymptomatic or cause sharp pain, dull aches, stiffness, and numbness in the affected heel. Corns and calluses also often form over the affected area. If you have painful heels, please see a podiatrist for a diagnosis and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Dean D. Hinners from Illinois. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Are You Suffering From Ingrown Toenails?
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Signs You May Have Developed Neuropathy
 Neuropathy is a condition that affects the feet, specifically causing them to lose feeling. This can be incredibly dangerous, especially if you have developed a serious foot condition and can not feel the symptoms of it. Neuropathy may also alter the shape of your foot. Your arch may be raised, your toes can begin to bend downward, and the bones at the ball of your foot may protrude outward. When the shape of the foot changes, it in turn changes its overall function as well. To keep your feet comfortable, you may want to look into wearing shoes with extra support. Other signs that indicate you may have developed neuropathy include sensations of numbness, stinging, burning, and stabbing aches and pains. Hypersensitivity, as well as dry or cracked skin may develop due to neuropathy. In order to receive a proper diagnosis, and a suggested plan for treatment, we recommend you consult with a podiatrist for professional care.
Neuropathy is a condition that affects the feet, specifically causing them to lose feeling. This can be incredibly dangerous, especially if you have developed a serious foot condition and can not feel the symptoms of it. Neuropathy may also alter the shape of your foot. Your arch may be raised, your toes can begin to bend downward, and the bones at the ball of your foot may protrude outward. When the shape of the foot changes, it in turn changes its overall function as well. To keep your feet comfortable, you may want to look into wearing shoes with extra support. Other signs that indicate you may have developed neuropathy include sensations of numbness, stinging, burning, and stabbing aches and pains. Hypersensitivity, as well as dry or cracked skin may develop due to neuropathy. In order to receive a proper diagnosis, and a suggested plan for treatment, we recommend you consult with a podiatrist for professional care.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Dr. Dean D. Hinners from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Understanding Athlete's Foot
 Athlete’s foot is a common fungal infection. A majority of athlete’s foot cases are caused by fungi that thrive in closed, warm, and moist environments. The fungi feed on Keratin, which is a protein found in the hair, nails, and skin. Athlete’s foot is mildly contagious and can spread through direct contact with the infection and by skin particles left on towels, shoes, or floors. Walking barefoot can increase the chances of contracting athlete’s foot. The risk can also go up depending on your susceptibility. People who have impaired immune systems or diabetes are at greater risk for infection if they have an open cut or sore on their foot. If you have developed athlete’s foot or feel that you may be at risk, it is advised that you consult with a podiatrist.
Athlete’s foot is a common fungal infection. A majority of athlete’s foot cases are caused by fungi that thrive in closed, warm, and moist environments. The fungi feed on Keratin, which is a protein found in the hair, nails, and skin. Athlete’s foot is mildly contagious and can spread through direct contact with the infection and by skin particles left on towels, shoes, or floors. Walking barefoot can increase the chances of contracting athlete’s foot. The risk can also go up depending on your susceptibility. People who have impaired immune systems or diabetes are at greater risk for infection if they have an open cut or sore on their foot. If you have developed athlete’s foot or feel that you may be at risk, it is advised that you consult with a podiatrist.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Dr. Dean D. Hinners from Illinois. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.