Featured Articles
Super User
Possible Causes of Bunions
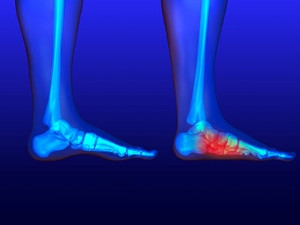
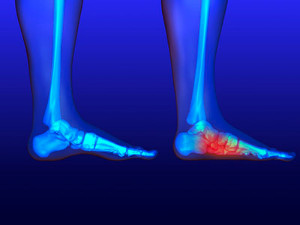
 Patients who have developed bunions are often aware of the pain and discomfort they may cause. A bunion appears as a bony protrusion on the side of the big toe, and it may be difficult to wear shoes. Some of the symptoms that are associated with bunions can consist of redness and swelling on the bottom of the big toe, and the second toe may overlap the big toe. Genetic factors may play a significant role in developing bunions, in addition to wearing shoes that do not have adequate room for the toes to move freely in. Some patients may have existing medical conditions that can increase the risk of obtaining a bunion, such as flat feet, or neuromuscular conditions. It may be beneficial to wear custom made orthotics which may help to relieve some of the pressure that bunions can cause. If you have developed a bunion, please consult with a podiatrist who can help you to manage this ailment.
Patients who have developed bunions are often aware of the pain and discomfort they may cause. A bunion appears as a bony protrusion on the side of the big toe, and it may be difficult to wear shoes. Some of the symptoms that are associated with bunions can consist of redness and swelling on the bottom of the big toe, and the second toe may overlap the big toe. Genetic factors may play a significant role in developing bunions, in addition to wearing shoes that do not have adequate room for the toes to move freely in. Some patients may have existing medical conditions that can increase the risk of obtaining a bunion, such as flat feet, or neuromuscular conditions. It may be beneficial to wear custom made orthotics which may help to relieve some of the pressure that bunions can cause. If you have developed a bunion, please consult with a podiatrist who can help you to manage this ailment.
If you are suffering from bunions, contact Dr. Dean D. Hinners of Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Are Flat Feet Painful?
 Factors that indicate you may have flat feet are often noticeable while standing on the floor. The arch of the foot will appear absent, or extremely low. The arch typically provides a spring to the step, and is helpful in distributing the weight of the body across the legs and feet. Flat feet may develop from birth, genetic factors, or from a possible foot or ankle injury. Common symptoms that can be associated with this condition may include foot pain, and the arch area may become swollen, as well as the calves. If you have flat feet, it is suggested that you are under the care of a podiatrist who can recommend specific stretching techniques. These may be helpful in alleviating some of the pain and discomfort that can come with this condition.
Factors that indicate you may have flat feet are often noticeable while standing on the floor. The arch of the foot will appear absent, or extremely low. The arch typically provides a spring to the step, and is helpful in distributing the weight of the body across the legs and feet. Flat feet may develop from birth, genetic factors, or from a possible foot or ankle injury. Common symptoms that can be associated with this condition may include foot pain, and the arch area may become swollen, as well as the calves. If you have flat feet, it is suggested that you are under the care of a podiatrist who can recommend specific stretching techniques. These may be helpful in alleviating some of the pain and discomfort that can come with this condition.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Dean D. Hinners from Illinois. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Do I Know If I Have a Plantar Wart?
 Plantar warts are small, rough, fleshy growths that can appear on the bottom of the foot. They are caused by the virus known as HPV and enter the body through a cut or break in the skin. Plantar warts typically appear at the base of the toes or on the heel. Their appearance is characterized by black pinpoints and a grainy texture. Plantar warts may cause pain when walking or standing, and can sometimes grow inwards, forming a callus. The wart might also cause lesions that can change the normal lines and ridges of the skin on the bottom of the foot. If you think you may have a plantar wart, it is suggested that you seek the care of a podiatrist.
Plantar warts are small, rough, fleshy growths that can appear on the bottom of the foot. They are caused by the virus known as HPV and enter the body through a cut or break in the skin. Plantar warts typically appear at the base of the toes or on the heel. Their appearance is characterized by black pinpoints and a grainy texture. Plantar warts may cause pain when walking or standing, and can sometimes grow inwards, forming a callus. The wart might also cause lesions that can change the normal lines and ridges of the skin on the bottom of the foot. If you think you may have a plantar wart, it is suggested that you seek the care of a podiatrist.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Dean D. Hinners from Illinois. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
The Dangers of Wearing Flip Flops

Many people enjoy wearing flip-flops during the warmer months. Their various colors and exemption of laces can make these types of shoes tempting to slip into. Research has indicated, however, that there may be some drawbacks to wearing flip-flops. Patients who frequently wear them may experience foot and ankle pain, in addition to walking differently. This may be a direct result of the flip-flops having no arch and little to no support. The toes must also work harder to keep these shoes on the feet. Additionally, flip-flop wearers often take shorter steps, and this can cause more stress to the overall body. Heel pain is also a common ailment among flip-flop wearers. Flip-flops generally have a thin sole and are backless, which can lead to the development of cracked heels. If you would like more information about the dangers of wearing flip-flops, please consult a podiatrist who can answer any questions you may have.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact Dr. Dean D. Hinners from Illinois. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Possible Causes of Flat Feet
 Patients who have flat feet are often aware of the absence of an arch. This is typically noticed while standing as the foot lies flat on the floor. The arch helps to balance the body’s weight between the feet and the legs and will generally determine a person’s walking style. People who have flat feet often notice their feet will roll inward or outward, and this is referred to as overpronation. The most common symptom that is associated with this condition is pain that is felt where the arch should be, and this may be a result of ligaments and muscles that have become strained. Existing medical conditions, which include arthritis or cerebral palsy may cause this condition to occur, in addition to genetic factors. If you have flat feet, it is suggested that you counsel with a podiatrist who can guide you toward proper treatment options.
Patients who have flat feet are often aware of the absence of an arch. This is typically noticed while standing as the foot lies flat on the floor. The arch helps to balance the body’s weight between the feet and the legs and will generally determine a person’s walking style. People who have flat feet often notice their feet will roll inward or outward, and this is referred to as overpronation. The most common symptom that is associated with this condition is pain that is felt where the arch should be, and this may be a result of ligaments and muscles that have become strained. Existing medical conditions, which include arthritis or cerebral palsy may cause this condition to occur, in addition to genetic factors. If you have flat feet, it is suggested that you counsel with a podiatrist who can guide you toward proper treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Dean D. Hinners from Illinois. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Lupus in the Feet
 Known as a chronic autoimmune disease, lupus and its symptoms are similar to that of arthritis, affecting the tissues in the joints and leading to various problems in the feet including bunions, claw toes, and hammertoes. Lupus can also lead to tendonitis, loss of feeling or neuropathy, muscle inflammation, corns and calluses, swollen feet or oedema, and more. It is especially important to watch lupus symptoms, as infections such as gangrene can develop in a healthy person. Visit your podiatrist to assess your condition, as well as invest in proper footwear with insoles.
Known as a chronic autoimmune disease, lupus and its symptoms are similar to that of arthritis, affecting the tissues in the joints and leading to various problems in the feet including bunions, claw toes, and hammertoes. Lupus can also lead to tendonitis, loss of feeling or neuropathy, muscle inflammation, corns and calluses, swollen feet or oedema, and more. It is especially important to watch lupus symptoms, as infections such as gangrene can develop in a healthy person. Visit your podiatrist to assess your condition, as well as invest in proper footwear with insoles.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Dr. Dean D. Hinners from Illinois. Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
Can Walking Help Poor Circulation?
 The medical condition that is known as poor circulation occurs when blood flow is restricted in the body. Common symptoms that are associated with this condition can include cold feet, in addition to a tingling and numbing sensation. This risk of developing poor circulation may increase as the aging process occurs. Other existing factors that can lead to this condition can include smoking, lack of exercise, and eating unhealthy foods. There are noticeable symptoms that are present if poor circulation exists. The most common sign is feeling cramps in your legs as you walk, and some patients are aware of consistent aches in their legs and feet. Mild relief can be obtained when a gentle walking program is implemented, and this can be helpful in controlling poor circulation. If you feel you have symptoms of this condition, it is suggested that you schedule a consultation with a podiatrist who can properly treat this condition.
The medical condition that is known as poor circulation occurs when blood flow is restricted in the body. Common symptoms that are associated with this condition can include cold feet, in addition to a tingling and numbing sensation. This risk of developing poor circulation may increase as the aging process occurs. Other existing factors that can lead to this condition can include smoking, lack of exercise, and eating unhealthy foods. There are noticeable symptoms that are present if poor circulation exists. The most common sign is feeling cramps in your legs as you walk, and some patients are aware of consistent aches in their legs and feet. Mild relief can be obtained when a gentle walking program is implemented, and this can be helpful in controlling poor circulation. If you feel you have symptoms of this condition, it is suggested that you schedule a consultation with a podiatrist who can properly treat this condition.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Dr. Dean D. Hinners of Illinois. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Where Is the Plantar Fascia?
 The portion of tissue that is found on the bottom of the foot is called the plantar fascia. It connects the heel to the toes, and helps to provide flexibility to the foot while walking and running. When this band of tissue becomes inflamed as a result of an injury or from overuse, the condition plantar fasciitis may develop. The symptoms that are generally associated with this condition can include severe pain and discomfort in the heel and surrounding area, and this pain may be worse in the morning after arising. Some patients find mild relief when the affected foot is rolled on a cold bottle, as this may be helpful in relaxing the affected muscles. If you suffer from plantar fasciitis, it is strongly suggested that you are under the care of a podiatrist who can properly treat this condition.
The portion of tissue that is found on the bottom of the foot is called the plantar fascia. It connects the heel to the toes, and helps to provide flexibility to the foot while walking and running. When this band of tissue becomes inflamed as a result of an injury or from overuse, the condition plantar fasciitis may develop. The symptoms that are generally associated with this condition can include severe pain and discomfort in the heel and surrounding area, and this pain may be worse in the morning after arising. Some patients find mild relief when the affected foot is rolled on a cold bottle, as this may be helpful in relaxing the affected muscles. If you suffer from plantar fasciitis, it is strongly suggested that you are under the care of a podiatrist who can properly treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Dean D. Hinners from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Metropolis and Eldorado, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.